3. Process Mapping
How to understand the repeat prescribing system
3.1 Process-mapping case studies
3.2 Process-mapping resources
There are many benefits of a robust repeat prescribing system.3
Benefits to patients and carers:
- The process is convenient, and patients can access the medicines they need in a timely manner
- There is a clear understanding and appreciation of the process
- Patients have confidence that they are receiving their medicines safely
- Patients are familiar with the purpose and importance of having a regular medication review and take the opportunity to share any issues, concerns and expectations related to their repeat medicines
- Patients are familiar with the purpose and importance of attending the practice for any required monitoring related to their repeat medication
- Patients are involved in decisions about their medicines and their care.
Benefits to practices:
- More streamlined, manageable workloads
- Reduced ‘failure demand’ through fewer queries and anomalous situations*
- Risks and safety issues can be better mitigated or managed
- More appropriate and efficient use of professional and practice staff time and skills
- Greater understanding of the process by everyone involved, including roles and responsibilities
- Improved communication and working relationships with other healthcare professionals, e.g. community pharmacy
- Easier implementation of other initiatives which can further reduce work burden and improve quality of care, e.g., eRD (see section 9)
- Reassurance and confidence for prescribers that the processes behind their clinical responsibilities are well-organised and robust.
*Failure demand is the demand caused by a failure to do something or to do something right for the customer.26 In a healthcare setting, failure demand describes the failure to get it right for the patient first time. Patients then come back, making further demands to resolve the issue, and thereby unnecessarily consuming practice or community pharmacy resources because the service they received was ineffective.
Benefits to the wider NHS:
- Assurance that medicines are used in a safe, effective and appropriate manner
- More efficient use of resources (including workforce) within the NHS
- Reduced medicines waste
- Reduced potential for adverse incidents and harm to patients
- Reduced potential for abuse of the repeat prescribing system.
Process mapping is a technique to visually map workflows and processes. It is a useful tool to enable practices to understand their own repeat prescribing process, which can be made of many separate procedures happening at the same time.
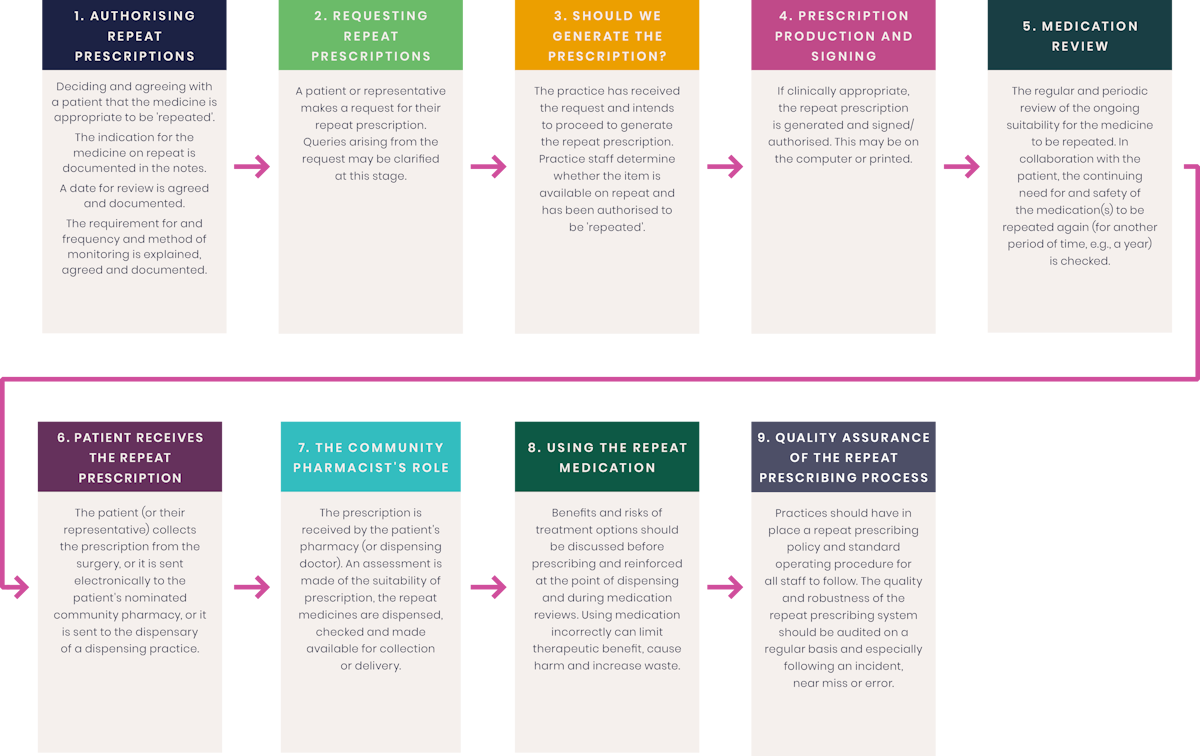
This concept was defined nationally in the 2004 National Prescribing Centre guidance and included a generalised repeat prescribing process map, illustrated in Figure 1.3 This resembles an underground rail network with a station marking each step, and some stations are common to different lines. This process map was published before the EPS or eRD were introduced.
It is important that each practice maps out their own local processes and overall system, ideally using protected learning time to do this as a collective group, with all members of the practice team represented and engaged – clinical, administrative and technical. Figure 2 shows some of the steps you may wish to include.
When undertaking process mapping, it is important to identify:
- Steps that are working well, and you want to keep
- Steps that are not adding value (or not improving safety) as these could be designed out of the new process
- Steps that could work better with a better process design. These could improve efficiency, safety or just make things simpler
- Where there are gaps in the process
- How escalation routes work, e.g., if requests need to move to a clinician
- Where a digital solution or clinical system functionality can be used to automate or simplify the step process
- Which role in the practice has the responsibility for completing each step, and consider if that is the most appropriate role.
Figure 1 - A map of the main elements of the repeat prescribing process
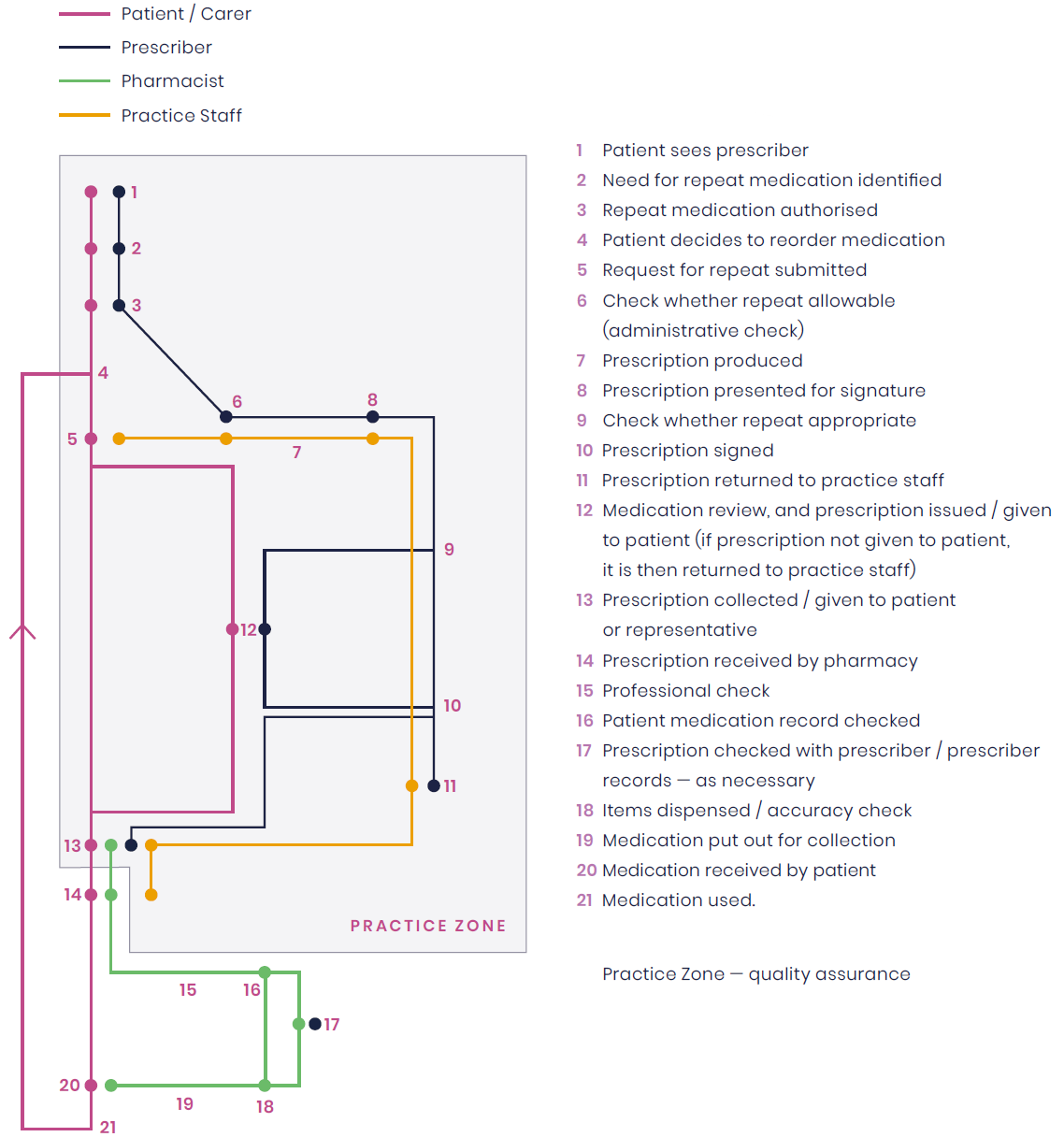
Figure 1 – NPC. ‘Saving time, helping patients – a good practice guide to quality repeat prescribing’ 2004 (archived).
Reproduced with permission from NICE.
3.1 Process-mapping case studies
These case studies, available on the NHSE website (general practice case studies) showcase where process mapping and redesign have improved efficiency, reduced clinician and practice team time spent on repeats and improved patient satisfaction and safety.
Case study summary
168 GP appointments released a month after redesigning the repeat prescription and medication review process
A practice in Staffordshire with a patient population of over 11,800 carried out a process-mapping exercise of the different steps it took for the practice to deal with medication requests and reviews. They involved the whole practice team to ensure accurate and complete input.
Understanding where time was wasted and identifying issues with the current repeat prescribing processes helped get all staff on board to support the changes for improvement that the group put forward. All the staff engaged in understanding the problems with the current processes and proposed solutions. Patients were engaged and involved in the process.
Key impacts:
- Over 28 hours of GP time released per month
- 42 hours of reception team’s time released per month
- Patients benefited from a streamlined approach for medication reviews, better availability of appointments and improved patient experience.
Case study summary
Dispensary and administration/reception teams working together to release 55 hours per week
A practice in Surrey working across two sites, including a dispensary, were struggling with high repeat prescription demand, and wanted to develop a more efficient process to release staff time.
Both site teams listed all the tasks involved in their repeat prescribing process and the essential steps that were frequently not completed. 35% of dispensary tasks were missed, this included tasks relating to controlled drugs. 39% of administrative/reception jobs were missed, e.g., booking appointments for patients that need a medication review. The heavy workload meant the team were in reactive mode and unable to plan a better approach.
By completing a skills matrix of current staff, this highlighted where standard operating procedures (SOPs) needed to be updated. Process mapping helped the team to objectively query every step to identify waste and value/non-value-adding work. Following testing, the teams reported back positively on the new process and the changes made.
Key impacts:
- Approximately 11 hours per day of dispensary and admin/reception teams’ time was released across both sites
- Time released is improving the service provided at the dispensary, including more time for face-to-face contact with patients, staff training and supervision
- The admin/reception team are now more able to work on patient and practice operational improvements including staff training, patient education and signposting
- Patients feel reassured, supported and better informed.
Case study summary
Re-designing the annual patient review process
Two practices came together under a single organisation to redesign the annual medication review process and deliver a common approach across both sites.
Staff did not have a clear understanding of the process from start to finish. Reviews took place on an ad hoc basis, often initiated/requested by the clinicians. There was a significant lack of clarity regarding responsibilities and poor communication. Clinicians were unsure of the reception team’s role in the process and vice versa.
They used what was currently working well for each team along with ideas of different and more efficient ways of working and incorporated them into the new process. At every stage, there was discussion and consultation with the wider practice teams and staff were given the opportunity to feedback and contribute to the changes being considered.
A single review process is now operating across both sites.
Key impacts:
- On course to achieve collective goal of over 3,100 reviews per year, leading to better patient monitoring
- Collaboration has improved understanding of others’ roles and responsibilities and enhanced further joint working
- Patients are receiving a more proactive service and saving time by scheduling all relevant review appointments during one medication review appointment.
3.2 Process-mapping resources
The NHS has useful resources to support process mapping and the Primary and Community Transformation and Improvement team, which was introduced as part of the delivery plan for recovering access to primary care, can provide tailored support for practices to make changes and improvements to how they work.
Their website includes webinars, guides and other support.
The Primary Care Improvement Connect Future NHS Platform also contains a wealth of resources to support practices with quality improvement methodology and case studies.
Practical actions that general practices might consider include:
- Completing a skills matrix to map out current skills, strengths and weaknesses in the team – an example skills matrix template can be found on the improvement team website to help understand who in the team is trained to manage prescription requests and identify where further training is required
- Align patient medication review dates
- Introduce eRD where it is clinically appropriate. Benefits are particularly seen for those patients with stable conditions and medications, e.g., levothyroxine, and their medication review can be aligned to long-term condition checks. For more information on eRD, see section 9
- Work closely with local pharmacies around changes being undertaken (reducing unnecessary calls, emails, etc.)
- Seek the views of your patients via the PPG. See questions for the PPG in section 5.4
- For patients who choose not to use the NHS app to manage their medications, look to optimise other digital channels (e.g., practice websites) to improve their ordering experience and streamline their requests in an appropriate workflow (recognising that digital solutions will not be suitable for all patients)
- Practices should discuss their arrangements for the minority of patients who are unable to use the usual repeat prescription ordering arrangements. This may be because they cannot access or use the NHS app (or other digital ordering arrangements) or because of chaotic lifestyle arrangements such as those caused when a person is homeless. Practices could consider assigning responsibility for managing these patients to a care co-ordinator (or similar) so that the arrangements support the patient and are efficient for the practice team
- Review the practice process for urgent repeat prescription requests and the reconciliation process if a request for a repeat medicine has been managed via NHS 111. See section 9.5 for emergency supply requests
PCNs provide an opportunity for constituent practices to collaborate in a wide variety of ways, including reviewing, developing and sharing repeat prescribing protocols to support more consistent arrangements.
Figure 2 - Repeat Prescription flow diagram