
Above: Sarah, Pharmacist, joins the Frailty Consultant led MDT
By Amanda Powell, Lead Pharmacist, Frailty/CRTs Aneurin Bevan UHB and Sally Lewis, Clinical Pharmacy Technician, CRTs/Intermediate Care Aneurin Bevan UHB

Across Wales, pharmacy teams are playing a vital role in supporting A Healthier Wales – helping patients stay well at home and ensuring continuity of care across health and social services.
At Aneurin Bevan University Health Board, our intermediate care pharmacy service has grown from a small pilot into a region-wide model supporting frail and elderly patients across Gwent. Our work demonstrates how collaboration, skill mix and innovation in clinical pharmacy can deliver better outcomes for patients and strengthen multidisciplinary team (MDT) working.
How our service began and developed
Our intermediate care pharmacy journey began in 2019 with two pharmacist posts and one and a half pharmacy technician posts. Today, thanks to investment through the Welsh Government Regional Integration Fund (RIF), the team has grown to 14 whole-time equivalent posts, spanning bands 3 to 8B. This growth reflects our success in delivering outcomes that align with the Welsh Government’s ‘A Healthier Wales: our Plan for Health and Social Care’. We have established pharmaceutical support across the five local authorities in the Gwent Region of South East Wales.
Our work includes:
- Frailty Consultant led virtual wards (Hospital at Home)
- Community Falls service
- Nursing IV administration at home including bone health and antimicrobial therapies
- Reablement service
- Post discharge follow up to ensure patient adherence and understanding.
We believe in increasing the value medicines bring to patients’ lives, rather than focusing on cutting costs.
Expanding continuity of care
The latest increase in funding allowed us to develop a pharmacy technician-led service in rehabilitation wards within our community hospitals. These sites are located close to our virtual ward bases, helping improve continuity of care as patients move between hospital and home.
This newly transformed pharmacy service focuses on deprescribing, falls prevention, assessing bone health and keeping patients familiar with their medicines regimes.

Above: Rhys, Pharmacy Assistant, explains Medicines Reminder Chart
Pharmacy Technicians as core members of the MDT
Our pharmacy technicians are fully integrated within consultant led MDTs, working at the top of their licence. with and without a pharmacist present. Being fully emersed in the MDT – sometimes independently of a pharmacist - allows all members to share and gain knowledge and experience from each other and our Pharmacy Technicians have developed at pace due to this exposure.

We have also developed a bespoke training programme and competency framework for the pharmacy technicians working within the Frailty service. Topics include:
- Renal function, U&Es and drug management
- Drug interactions
- Anaemia
- Bone Health
- Anticoagulation
- Antimicrobial stewardship
- Management of COPD
- Management of Heart Failure
- Deprescribing and Medicines Optimisation
When faced with an unfilled pharmacist vacancy recently, we opted to recruit an extra pharmacy technician instead. This decision reflects our belief in building a future where pharmacy technicians are empowered as registrants making clinical decisions and referring on appropriately when needed.
Next steps – making every contact count
Our team are always developing. One of our pharmacists now attends a Frailty Heart Failure clinic with a specialist nurse and consultant. As our Hospital at Home service includes a high proportion of patients with heart failure, the continuity of care is increased through this initiative – something so important for this cohort of patients.
We are also collaborating with GP practices in another locality to carry out proactive pharmacy visits to the frail elderly patients. This approach helps us identify those most in need of support, ensuring they receive the right care in the right place. Not enough pharmacy colleagues see patients in their homes and we are keen to expand this work with colleagues across our health board.
We are also exploring how Medicines Reminder Charts can help patients remain independent with their medicines. A template integrated into community pharmacy dispensing systems would make this easier to use in practice.
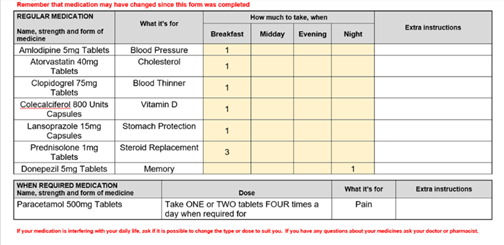
Example Medicines Reminder Chart
Finally, we would like to work more closely with community pharmacy colleagues to increase early intervention for falls prevention, optimise bone health and raise awareness of ‘sick day rules’. We feel that these are some of the main reasons for frail, elderly patients coming into hospital.
Our journey is ongoing, and we still have so much to achieve for our patients.
Read more RPS blogs.